- Details
- Written by: Naomi Harrison
- Category: News
- Hits: 492
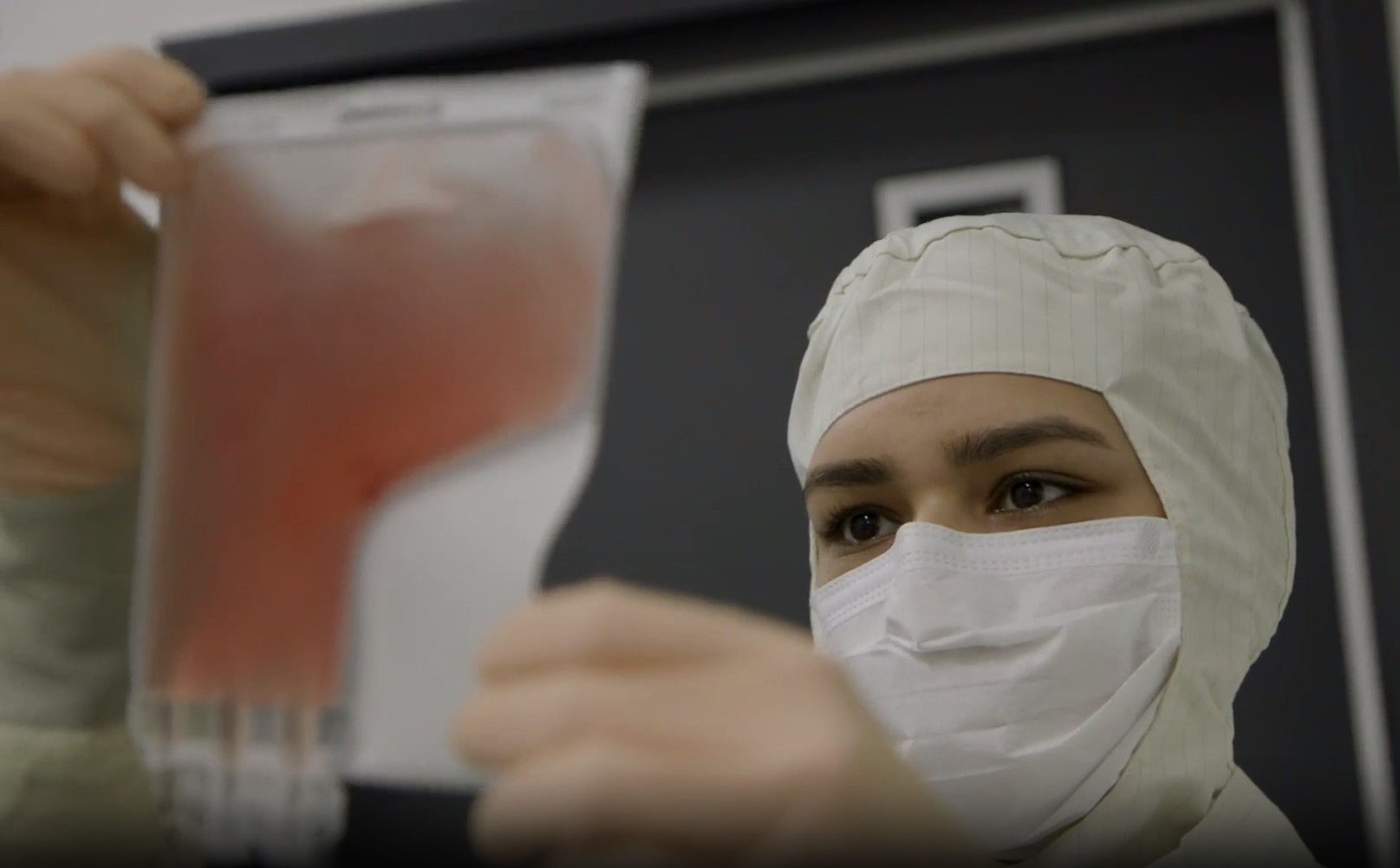
An international clinical trial involving many Peter Mac patients has shown that CAR T-cell therapy provides significant benefits compared to standard treatment of relapsed multiple myeloma.
This CARTITUDE-4 study compared Janssen’s “Cilta-cell” CAR T-cell therapy to standard therapies in patients whose myeloma had returned despite up to three earlier forms of treatment.
Peter Mac was the leading Australian recruitment site for this pivotal Phase III clinical trial which involved 81 hospitals globally - mostly in the US, Europe and Asia.
In all, 419 patents were enrolled and randomised to receive either CAR T-cell therapy or their next standard-of-care treatment.
Patients in the CAR T-cell therapy group were more likely to show an early and deep “complete response” - meaning their blood cancer became undetectable – at 73% compared to 22% for standard-of-care.
And, after one year, progression free survival in the CAR T-cell therapy group was 76% compared to 49% for standard of care.
These results have just been presented at the American Society of Clinical Oncology (ASCO) conference in the US, plus in corresponding paper in the New England Journal of Medicine.
Professor Simon Harrison, Director of the Centre of Excellence in Cellular Immunotherapy and a leading Haematologist in the Myeloma team at Peter Mac, led the trial in Australia.
“Not only was CAR T-cell therapy more likely to produce rapid and deep initial responses in patients, most of whom had heavily pre-treated myeloma, these responses were also usually more durable than those resulting from standard of care,” says Prof Harrison.
“CAR T-cell therapy represents a significant treatment advance for myeloma, a blood cancer which is still considered to be incurable, with these results even more impressive than those for the MSAC approved CAR T-cell therapies for B-cell acute lymphoblastic leukaemia and aggressive lymphoma.
“These results, following on from those from the CARTITUDE-1 study, will lead to a change the treatment paradigm for patients with myeloma.”
The NEJM paper is titled “Cilta-cel or Standard Care in Lenalidomide-Refractory Multiple Myeloma”.
- Details
- Written by: Naomi Harrison
- Category: News
- Hits: 478
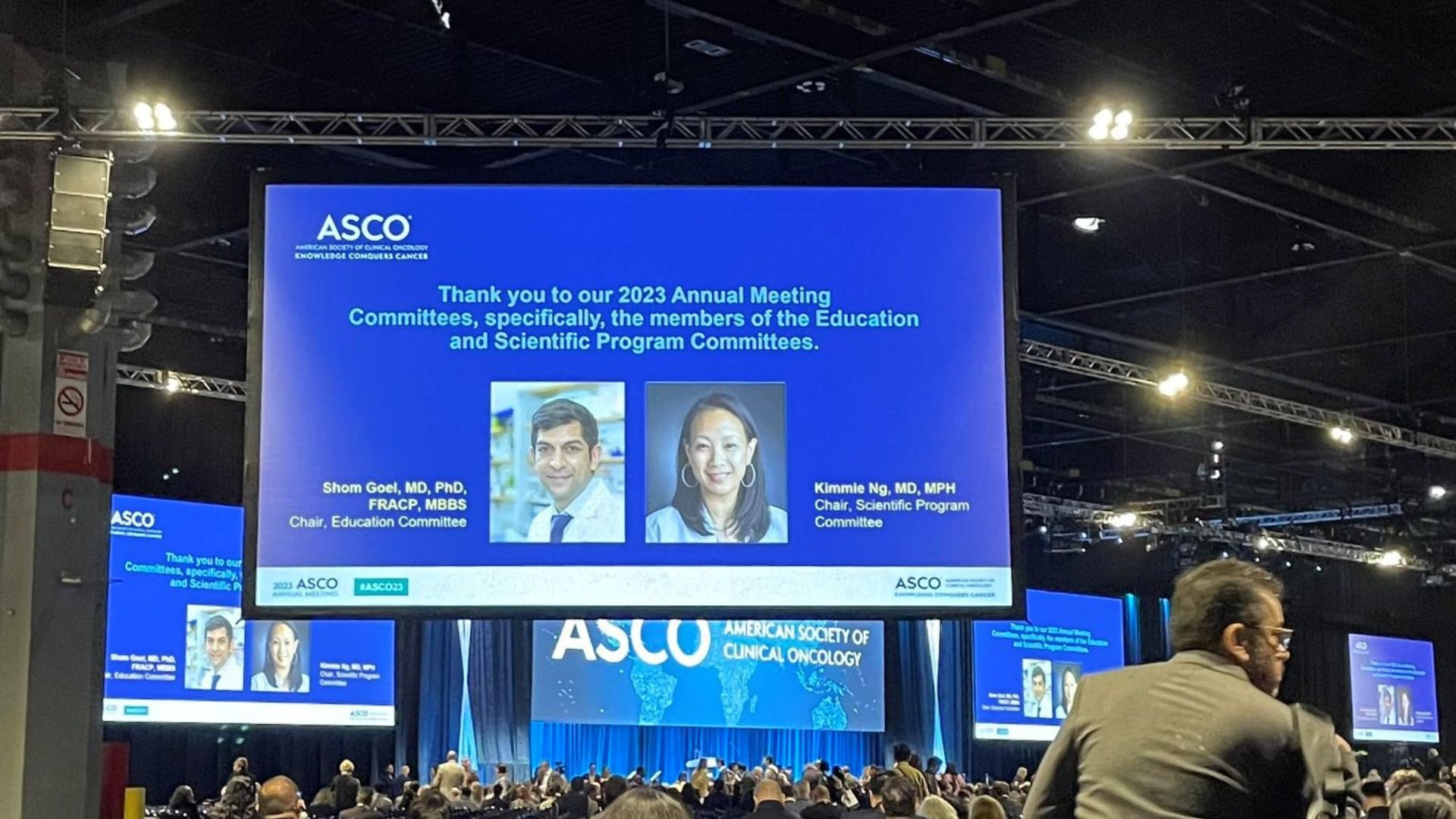
Peter Mac researchers have played a leading role at the weekend’s American Society of Clinical Oncology (ASCO) Annual Meeting in Chicago.
ASCO is considered the most important and prestigious meeting in the world of oncology with over 42,000 delegates attending.
Peter Mac’s Associate Director, Clinical Research, Professor Jayesh Desai, said the event was an opportunity to hear from the world’s best clinical researchers.
“In a huge honour, our own Professor Shom Goel was the Chair of the Education Committee for the 2023 Annual Meeting working with the ASCO President, faculty and staff to create the entire education program,” Prof Desai said.
“This is the first time a person outside of North America has been tasked with this responsibility and speaks to the high regard Professor Goel is held in by world leaders in cancer research,” he said.
“It was also wonderful to see Professor Ben Solomon’s expertise in Lung Cancer recognised through his role as an invited discussant for the Plenary session.”
A discussant is responsible for providing professional and constructive criticism and raising issues for broader consideration during the session. Discussants are experts in the area drawing upon their knowledge when commenting on papers or presentations.
“This was a huge honour for Professor Solomon and a reflection that his global peers see him as an insightful leader in the field of lung cancer,” said Prof Desai.
Peter Mac also had numerous clinician researchers invited to share their expertise and knowledge as speakers in educational sessions these included, Jeanne Tie, Ben Solomon, Grant McArthur, Jayesh Desai, Shom Goel, Michael Jefford and Dr Naomi Katz.
Associate Professor Shahneen Sandhu also presented a first in human trial conducted at Peter Mac to determine if an already approved treatment will make radioactive treatment Lu-PSMA-617 more effective at killing prostate cancer cells. Dr Lauren Brown presented both a poster and an oral presentation on her research in early breast cancer. Her abstract received an ASCO Merit Award for an outstanding abstract. Only four percent of all abstracts submitted are chosen for oral presentation demonstrating the high calibre of this research.
Professor Sherene Loi and Associate Professor Ben Tran were invited to discuss abstracts presented during a breast cancer clinical science symposium, and the genitourinary cancer – prostate, testicular and penile session respectively.
Professor Michael Jefford’s expertise and knowledge in survivorship was also acknowledged with Michael discussing how to assess and meet the needs of survivors and providers in a Meet the Professors session.
Aside from the important role Professor Shom Goel played as the Chair of the Education Committee, several people from Peter Mac were involved in planning committees. These included Professors Linda Mileshkin, Michael Jefford, Jayesh Desai and Associate Professor Shankar Siva.

- Details
- Written by: Naomi Harrison
- Category: News
- Hits: 743
Monash University and the Peter MacCallum Cancer Centre will drive forward world-class cancer research while training the next generation of clinicians and scientists, with a new partnership agreement now in place.

As Australia’s leading Comprehensive Cancer Centre focused on cancer care, research and education, Peter Mac will collaborate more closely with Monash University across all forms of research – in laboratories, clinics and for health services research initiatives.
The partnership will also enable more Monash University undergraduate, honours and post-graduate students to access research and clinical placements, as well as other supervised education opportunities at Peter Mac. The renewed and refreshed Affiliation Agreement was officially signed on Wednesday 7 June, building on a previous agreement that has been in place since 2017.
The agreement recognises the strengths of Monash University, which is ranked in the world’s top 50 universities in the 2023 Times Higher Education World University Rankings, while acknowledging Peter Mac’s unique role as Australia’s only public health services dedicated to caring for people with cancer.

Peter Mac Chief Executive Professor Shelley Dolan said the Affiliation Agreement was a significant step that would accelerate the achievements of these two leading organisations.
“We are delighted to embark on this expanded partnership with Monash University, which reflects the strong collaborations that our people have shared for many years,” Professor Dolan says.
“Working together helps both organisations to progress our shared goals of advancing cancer treatment and research, and of building a bigger and more equipped healthcare workforce in Victoria.”
Monash University Executive Dean, Faculty of Medicine, Nursing and Health Sciences Professor Christina Mitchell AO said: “Innovative, new ideas that have the greatest potential to advance cancer research and improve clinical outcomes are possible when the brightest minds in basic lab-based research work closely with talented clinicians.”
“This collaboration has the potential to accelerate the pace of cancer research by bringing teams together from two great institutions.”
The Affiliation Agreement, which is in place for at least five years, prioritises areas of mutual leadership to enable breakthroughs on future treatment and models of patient care, while ensuring Victoria and Australia more broadly, is home to a strengthened, future-ready health system.

- Details
- Written by: Naomi Harrison
- Category: News
- Hits: 269
New Peter Mac research recently published in Proceedings of the National Academy of Sciences (PNAS) has discovered a fundamental breakthrough related to the development of liver cancer

The research team, led by Dr Andrew Cox and Dr Kristin Brown, were motivated to understand how the KEAP1-NRF2 pathway - identified as one of the top 10 driver pathways in cancer - contributes to the initiation of liver cancer.
They found that mutations in the KEAP1-NRF2 pathway rewire metabolism by increasing the number of lysosomes in the cell. In healthy settings, lysosomes provide an important function to break down and dispose of damaged materials in the cell. However, in a cancer setting, lysosomes have been found to contribute to tumour progression.
“It was through a combination of unbiased approaches that we came across the relationship between the KEAP1-NRF2 pathway and lysosomes,” Dr Brown said.
“We know that lysosomes make cancer cells grow even more out of control than they normally would and that they contribute to the development of therapy resistance.
“We're very excited about this research. We think there is huge potential with respect to understanding why liver cancer develops and how we can better treat patients diagnosed with this disease.
“It is incredibly important that we find out how lysosomes are regulated so that we can develop new cancer therapies in the future.”

With the incidence of liver cancer increasing and few existing therapeutic options to treat this disease, Dr Cox added that it’s therefore critical to understand the processes driving liver cancer development.
“The KEAP1-NRF2 pathway plays an important role in protecting healthy liver cells from oxidative stress,” he said.
“Curiously, this pathway is mutated in a variety of cancers, including liver cancer. Our discovery that KEAP1-NRF2 pathway activation increases the abundance of lysosomes provides important fundamental insights into liver cancer development.”
This important collaborative work was carried out in the Cox and Brown labs and driven by PhD student Athena Ong, who is now working as a postdoctoral researcher at Peter Mac.
“Athena has already initiated follow-up studies to look more in depth at the role of the lysosome in liver cancer,” Dr Brown said.
This research was conducted with the support of the Peter Mac Foundation (Ted and Lila Seehusen Foundation). You can read the paper in full via the PNAS website.

- Details
- Written by: Ashley Hibbert
- Category: News
- Hits: 151
Peter Mac researchers have found the answers to cancer survivability may lie in the stars.

The latest research, published in Nature Communications this week, has shown that techniques initially developed for astronomy and ecology can be used to study the microenvironment of solid tumours.
Led by Peter Mac’s 2020 Lea Medal winner Dr Anna Trigos (pictured above) and Yuzhou Feng, the study looked at patient tumour samples from prostate, colon and breast cancers and identified novel cancer subtypes, new patterns associated with patient survival, and was able to predict which patients were likely to develop metastasis first.
These exciting results have generated significant interest from medical oncologists, pathologists and immunologists.
“Many novel treatments are constantly being developed, but it is challenging to know what treatment will be best for a particular patient,” Dr Trigos said.
“As a result, some patients receive treatments that will not work for them, losing valuable time and missing out on better options.
“We investigated new ways in which doctors can predict whether a treatment will work in a particular patient, but rather than looking at specific genes, we analysed tumours as if they were a cosmos – looking at the location of millions of individual cells much like stars in the universe.”
Tumours are composed of millions of cells, including immune cells (that help fight infection), fibroblasts (that hold the tissue together) and endothelial cells (that make blood vessels).
This study found that there are certain patterns, or predictable ‘ecosystems ‘, in how cells in a tumour are located, much like constellations in our universe. The Peter Mac team found these patterns can then be used to predict how patients might respond to treatment or determine how aggressive a cancer is.
The researchers developed a computational toolkit called SPIAT (Spatial Image Analysis of Tissues), which can derive and quantify these patterns.
“As a result, these methods are being included in studies of clinical trials investigating response to novel treatments,” Dr Trigos said.
“We believe that the cell types present and how they are located relative to one another is key in determining whether a cancer grows and whether a treatment will be effective.
“This is an exciting development as our strategy has provided a way to finally measure these patterns and relate it to patient outcomes.”
This successful Peter Mac research was funded by the National Health and Medical Research Council Ideas grant.
