- Details
- Written by: Naomi Harrison
- Category: News
- Hits: 98
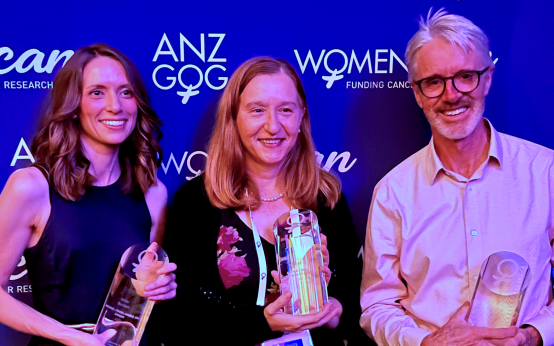
Three Peter Mac staff were recognised with prestigious awards at the Australia New Zealand Gynaecological Oncology Group (ANZGOG) Annual Scientific Meeting overnight.
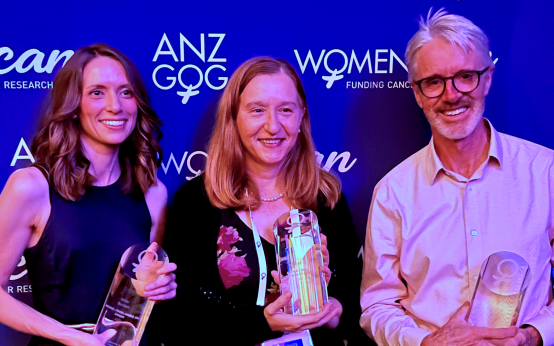
The awards highlight the outstanding contributions to improving life for women through cancer research.
Congratulations to the following winners:
-
Professor Linda Mileshkin was awarded the Clinical Trial Achievement Award in recognition of her significant contribution and leadership in research in gynaecological cancers.
-
Professor David Bowtell received the ANZGOG Research Pioneer Award for his consistent innovation in ovarian cancer research.
-
Dr Nikki Burdett was the winner of the Michael Friedlander Early Career Researcher Award for an outstanding early career researcher, with Dr Burdett recognised as one of the future leaders of ANZGOG.
ANZGOG is the peak gynaecological cancer clinical trials organisation for Australia and New Zealand. Its purpose is to improve outcomes and quality of life for women with gynaecological cancer through conducting and promoting cooperative clinical trials and undertaking multidisciplinary research into the causes, prevention and treatments of gynaecological cancer.
Peter Mac is proud to have three researchers recognised for their outstanding work and commitment to making a difference.
Congratulations Prof Mileshkin, Prof Bowtell and Dr Burdett!

- Details
- Written by: Naomi Harrison
- Category: News
- Hits: 174
Patients at Peter MacCallum Cancer Centre will soon have access to increased care and support, with the creation of a new Enhanced Care Unit (ECU).
Acute Care Specialist, Dr Ian Richardson, said the new six-bed ward would provide additional monitoring and care for cancer patients with more complex needs.
“The Enhanced Care Unit is not a substitute for Intensive Care but it fills a gap, allowing us to match patients with the most appropriate environment depending on their individual care needs,” Dr Richardson said.
“By offering this intermediate level of care, Peter Mac can safely care for higher acuity patients onsite while freeing up intensive care beds for patients who most need them.”
The Enhanced Care Unit, which has the support of the Victorian Department of Health, will be co-located with Peter Mac’s operating suite, with dedicated medical, nursing, allied health and pharmacy staff. Recruitment is currently underway for each of these positions.
Dr Richardson, who has recently been in the UK and Europe reviewing high acuity models of care, said international examples have highlighted the benefit of the Enhanced Care Unit model.
“Some of our patients require a higher level of care than our medical and surgical wards are designed to offer, so we rely on our close relationship with the Royal Melbourne Hospital to ensure these patients are cared for safely,” Dr Richardson said.
“The establishment of an Enhanced Care Unit will provide a specialised environment that offers our patients another layer of monitoring and support without the need for them to be transferred to another hospital.
“This is an exciting announcement for patients and staff, and will help us deliver even better personalised care for our patients.”
Close monitoring following complex surgery is one of the main drivers of good patient outcomes and Peter Mac’s Enhanced Care Unit will give cancer patients at Peter Mac improved access to cardiorespiratory and cardiac support.
“The Enhanced Care Unit will help ensure our medical and surgical patients get the right level of care as quickly as possible, reducing the risk of complications after surgery as well as caring for unwell patients presenting for care at any time,” Dr Richardson said.
Explore roles in the Enhanced Care Unit.
For media enquiries, please contact the Peter Mac Communications team on 0417 123 048
- Details
- Written by: Naomi Harrison
- Category: News
- Hits: 129
Meet Peter Mac Medical Physicist Dr Price Jackson, whose job you may have never heard of.
Working in both a clinical and research capacity, Dr Price is integral to the safe running of much of Peter Mac’s radiation and imaging equipment.
Peter Mac’s Medical Physics team work across Radiation Oncology and Medical Imaging, with some staff members working on research projects and supporting clinical trials.
Describing his role, Dr Jackson says, “we’re the tech people who know how the equipment works. When there isn’t a turn-key solution, we set things up.”
Dr Jackson started at Peter Mac 10 years ago as a postdoctoral researcher, developing dosimetry processes for radio-nuclear therapies in neuroendocrine cancer. Dosimetry is the process of measurement, calculation and assessment used to calculate radiation dose.
Later, he stepped into a more clinical role, testing and running the machines in Radiology, explaining “It feels good when we’re here to help the doctors when they have an idea…saying ‘yes we can do that’ and being there to set up the machines for whatever they need.”
For the last five years Dr Jackson’s focus has been on building image analysis tools to compliment clinical trials. He is interested in the emerging role of artificial intelligence (AI), which is being used more and more for image recognition and data analysis in healthcare.
Programs can be trained by looking at previous scans, learning from them, then using image and pattern recognition to analyse future scans for differences and abnormalities. The idea is to improve the speed and accuracy of scan assessment for future patients.
Peter Mac has an AI Working Group, which for over a year has been bringing together staff working with AI together to collaborate, share resources to improve all of their programs.
Dr Jackson is a member of the group and said it’s about, “bringing together different teams that are working towards the same ends”.
Some current research in Medical Physics is using AI analysis tools to predict treatment responses to prostate therapies. Another uses AI to categorise dose responses in radiation therapy.
Not all research in the field of medical physics surrounds AI though.
Another medical physicist at Peter Mac, Associate Professor Nick Hardcastle is leading a team designing and manufacturing a chair for patients to receive their radiotherapy in – with the aim to provide a more comfortable treatment option and reduce collateral radiation doses.
He says it could even bring radiation treatment - which currently requires lots of physical space and expensive technology - into more regional and rural areas.

- Details
- Written by: Naomi Harrison
- Category: News
- Hits: 103
Nearly $4 million in grants have been awarded to three Peter Mac-led research projects through the Federal Government’s Medical Research Future Fund (MRFF).

The MRFF supports a range of research initiatives to discover new ways to diagnose, treat and care for people with a variety of health conditions.
The three successful Peter Mac-led projects involve an evidence-based approach to pharmacogenomic medicines optimisation in adult and paediatric cancer cohorts, implementing universal tele-prehabilitation into cancer care pathways, and improving optimal pain and symptom management for Australians affected by pancreatic cancer.
Executive Director Cancer Research, Professor Ricky Johnstone, said the MRFF grants are a wonderful outcome for Peter Mac research and our partner organisations.
“It’s incredible to see such strong support for research at Peter Mac from the MRFF,” he said.
“This research will help us to look at ways to improve outcomes and quality of life for cancer patients, and highlights the innovative work being done by researchers at Peter Mac and the quality of our research faculty.
“We thank the MRFF for their support and congratulate to Marliese, Linda and Mei on their grants.”
Read more about each project below.
Dr Marliese Alexander - PhaRmacogEnomiC medIcines optimiSatIon for peOple with caNcer
PRECISION is a multi-trial, multi-centre, mixed-methods program that will discover, translate, implement and evaluate an evidence-based approach to pharmacogenomic (PGx) medicines optimisation in adult and paediatric cancer cohorts.
Conducting two clinical trials and using implementation science methods, this research will assess feasibility, acceptability, needs, cost effectiveness and scalability of PGx-guided medicines optimisation to enable safer and more effective use of medicines for people with cancer.
Three program streams of clinical trials, implementation, and discovery will simultaneously investigate multiple clinical and research questions while focussing on confirming the feasibility of PGx in cancer care.
The project is in collaboration with Bendigo Health, Border Medical Oncology, Regional Trials Network Victoria (RTN-Vic), Murdoch Children's Research Institute, University of Melbourne, University of Adelaide, University of Newcastle, Royal Melbourne Institute of Technology, Monash University, MyDNATM and Illumina©.
Professor Linda Denehy - Implementing univerSal Tele-prehabiliTation into cAnceR caRe pathwayS trial (STTARRS)
A large number of major surgical procedures happen each year in Australia, predominately for treatment of cancer. Individuals with increased surgical risk are expected to grow three-fold over the next 30 years, adversely impacting both patient outcomes and healthcare budgets if this problem is not addressed.
The physiological challenge of major surgery has been likened to running a marathon. In both cases, preparation is critical. Yet, many patients embark on major surgery without understanding the potential consequences. Complications after surgery are strongly associated with poor patient recovery and increased healthcare costs.
STTARRS is a randomised multicentre clinical trial measuring the effects of delivering teleprehabilitation education by allied health and nursing clinicians for patients before major cancer surgery at several Australian hospitals. We call this intervention “Surgery School”. We will measure complication rates, length of hospital stay, as well as implementability and economic outcomes. If effective, STTARRS is readily scalable nationwide.
Professor Mei Krishnasamy - Overcoming inequity of opportunity for optimal pain and symptom management for Australians affected by pancreatic cancer
Patients with cancer have better quality of life and health outcomes when a specialist nurse is involved in their care. In Australia, there is considerable variation in access to specialist cancer nurses, especially for regional and rural patients and those diagnosed with less common cancers. This randomised clinical trial will test a centralised and consumer-informed model of nurse-led telehealth care to improve patient outcomes for patients with pancreatic cancer.
The centralised model of care will be based at Peter Mac and tested through collaboration with two regional sites. The intervention builds on foundational evidence generated by our team multidisciplinary cancer clinicians, health services researchers and critically, our consumer partners.
The study will generate evidence that supports translation of more effective nurse-led approaches to improve patient outcomes (pain and symptoms) through collaboration between consumers and clinicians.
The project is in collaboration with Bendigo Health, Border Medical Oncology, Western Health, The Australian Pancreatic Cancer Foundation – Pankind, Burnet Institute, VCCC Alliance, University of Melbourne, Centre for Health Economics Research and Evaluation, University of Technology (Sydney), Queensland Institute of Medical Research and University of Queensland.
Other collaborations:
Peter Mac is also collaborating on a further three projects awarded MRFF grants:
- Professor Michael Jefford is working with Deakin University on an interactive online portal (iCare) to improve health and wellbeing for people living with complex cancers
- Professor Simon Harrison and Associate Professor Jane Oliaro are partnering with WEHI on a novel stem cell-derived manufacturing platform for next-generation dendritic cell vaccines
- Mark Xiang Li is teaming up with St Vincent’s Institute (SVI) to explore repurposing approved drugs for Friedreich’s ataxia heart disease.
Peter Mac is proud to receive these MRFF grants and look forward to advancing our management of cancer with this vital funding.

- Details
- Written by: Naomi Harrison
- Category: News
- Hits: 224
In an Australian first, a Peter Mac patient has had his melanoma zapped with targeted electrical pulses – helping to deliver chemotherapy deep inside cancer cells.

During the procedure on Friday morning - known as electroporation - chemotherapy was injected directly into the tumour on the patient’s head, followed by small electrical pulses delivered by a device that looks like a large pen.
“The electrical pulses make temporary holes in the cell membrane, allowing the drug to penetrate deep inside before the membrane seals off,” Peter Mac’s Dr Hayden Snow, who undertook the procedure said.
“With the chemo inside the cancer cells, they then hopefully start to die back and the tumour will start to shrink over the coming weeks.”
“It’s possible that a single dose is all that’s needed to kill the tumour, but additional treatments can be delivered in the future if required.”

The 20-minute electroporation procedure, done under a local anaesthetic, is a possible alternative to surgery – which would require multiple wounds and skin grafts – and radiation therapy, which would see daily treatments over a number of weeks.
It also delivers the chemotherapy locally, directly to the tumour – rather than it being delivered in a conventional way that affects the whole body.
The patient will likely be left with only a small amount of scar tissue – a far less visible reminder of the cancer versus surgery with a skin graft.
“It’s really exciting to be able to deliver such targeted treatment with minimal impact on the patient – he can head home today and will need very little down time,” Dr Snow added.

Dr Snow was assisted during the procedure by Professor Jim Clover, a consultant plastic surgeon from Cork University Hospital - who is in Australia for the launch of the treatment machine at a melanoma conference next week.
He has seen promising results treating skin cancer cancers in Europe with the technology over the past few years.
“Broad figures are that we would expect four-out-of-five lesions treated to respond, with three-out-of-five responding completely,” Professor Clover says.
“When you compare that to some of the other treatments that are available, they have effectiveness rates of probably half of that. So for targeted areas it’s a really powerful tool.
“And the key thing is to have the biggest toolbox possible when treating skin cancer.”
Health device company Endotherapeutics has brought the technology to Australia and hopes it will “add to the current standard of care” and improve patient experience.
