- Details
- Written by: Nadia Joulian
- Category: News
- Hits: 208

Peter Mac researchers have uncovered how to potentially stop head and neck cancer from spreading by “flicking a switch” and putting it back into growth mode.
Research led by Dr Charbel Darido and his team found that head and neck cancers can either grow or metastasise (spread to other parts of the body) - but not both at the same time.
They compared the behaviour of individual cells that were on the edge of a tumour and ready to spread, to those cells that were growing and dividing.
“Our research showed that when cells were reactivated and could continue to grow, they were no longer able to spread and invade other parts of the body,” Dr Darido explains.
“This discovery and concept could be seen as quite controversial in the science community because we usually want to stop the growth of tumours not promote the growth. But in this case, growth can be helpful.
“Most head and neck cancers become aggressive and stop responding to treatment when they spread to other organs, so we really want to try and to prevent this from occurring,” Dr Darido said.
The long-term aim of this discovery is to treat advanced stage head and neck cancers, keeping the size of the tumour under control and preventing it from spreading around the body and becoming untreatable.
More than 660,000 new cases of head and neck cancers are diagnosed worldwide with over 325,000 deaths every year.
The research conducted by Dr Darido and his team at Peter Mac was published in Nature Communication at the end of March 2023.
- Details
- Written by: Nadia Joulian
- Category: News
- Hits: 202
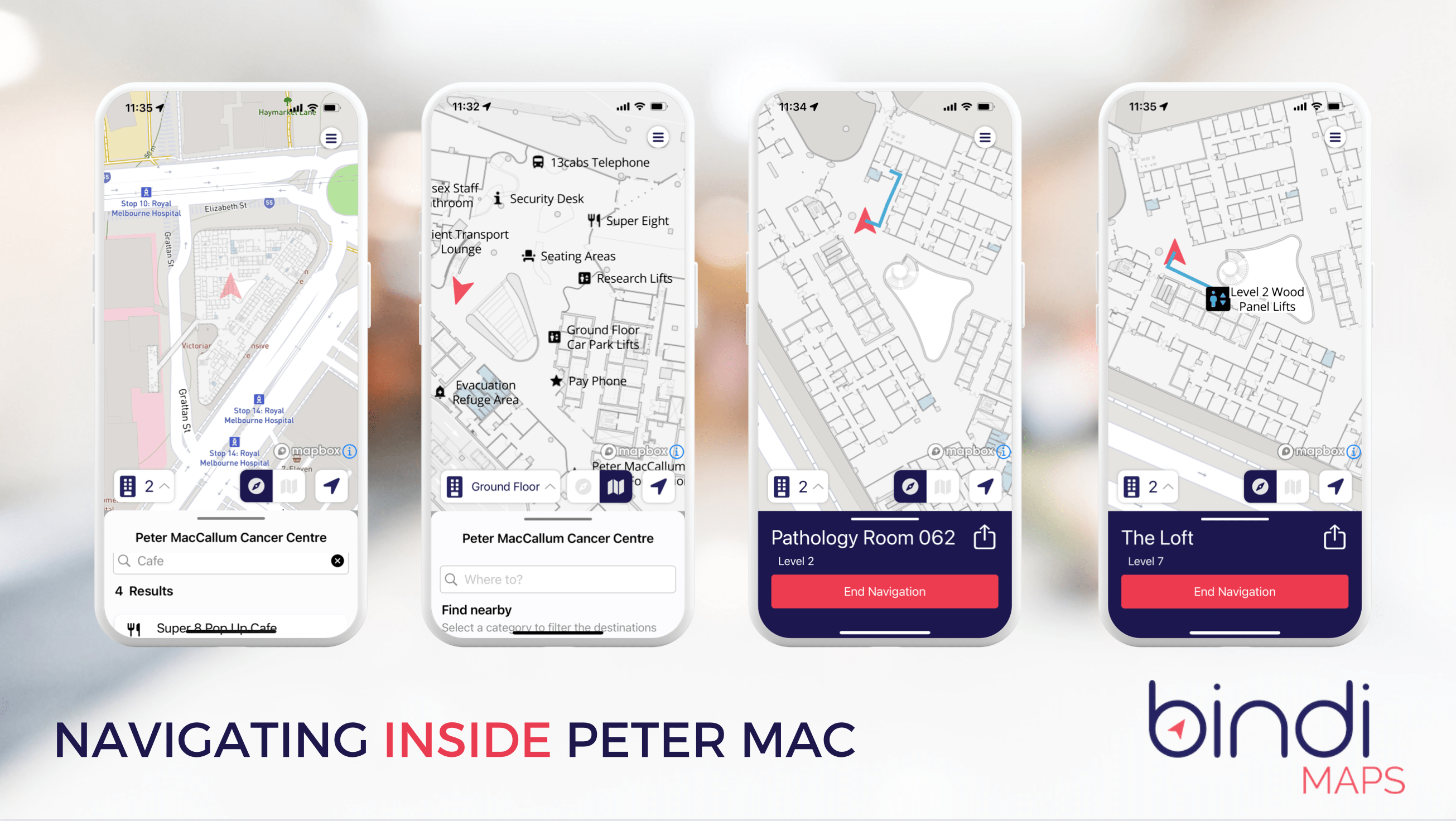
The Peter MacCallum Cancer Centre in Parkville has become the first hospital in Victoria to make life easier for vision impaired patients and visitors by installing a new wayfinding system - BindiMaps.
The ‘BindiMaps’ app will help those who are visually impaired navigate their way around some of the key public spaces at Peter Mac via audio instructions that describe where they are, what’s around them and the best way to get to their destination.
Peter Mac Chief Medical Officer Dr David Speakman said the new system is designed make life easier for vision impaired patients and visitors coming to Peter Mac.
“We know how challenging it can be to receive a cancer diagnosis or to visit someone in hospital with cancer, especially for those who are visually impaired,” Dr Speakman said.
“This new system will provide an additional level of support to people coming to Peter Mac and allow them to find their way around our Parkville campus by following clear and detailed audio directions via an app on their phone.
“The app connects with beacons that have been installed in different areas around our Parkville building and provides audio updates to users to let them know where they are, as well as directing them to where they need to go.
“It’s particularly designed to assist the vision impaired but is available to help anybody who downloads the app to access some of the key areas at Peter Mac,” he said.
The project was driven in part by the Peter Mac Consumer Advisory Committee with input from vision impaired consumers like Kevin Boyce.
Kevin’s mother received cancer treatment at Peter Mac.
“More than 20% of patients who use the Victorian health system have a disability,” Kevin said.
“Having access to the BindiMaps system at Peter Mac will make life far simpler for patients who are visually impaired or have other disabilities, as well as assisting visitors and family members who also need to navigate a busy hospital,” he said.
BindiMaps CEO, Anna Wright said hospitals are large and complex buildings that can present a daunting set of wayfinding challenges.
“Having BindiMaps installed at Peter Mac will help everyone to find their way around including patients and visitors with low or no vision, and those who prefer wheelchair accessible options,” Anna said.
The BindiMaps service will be ‘switched on’ at Peter Mac from Thursday 27 April and the app can be downloaded free of charge from App Store and Google Play.
- Details
- Written by: Nadia Joulian
- Category: News
- Hits: 116
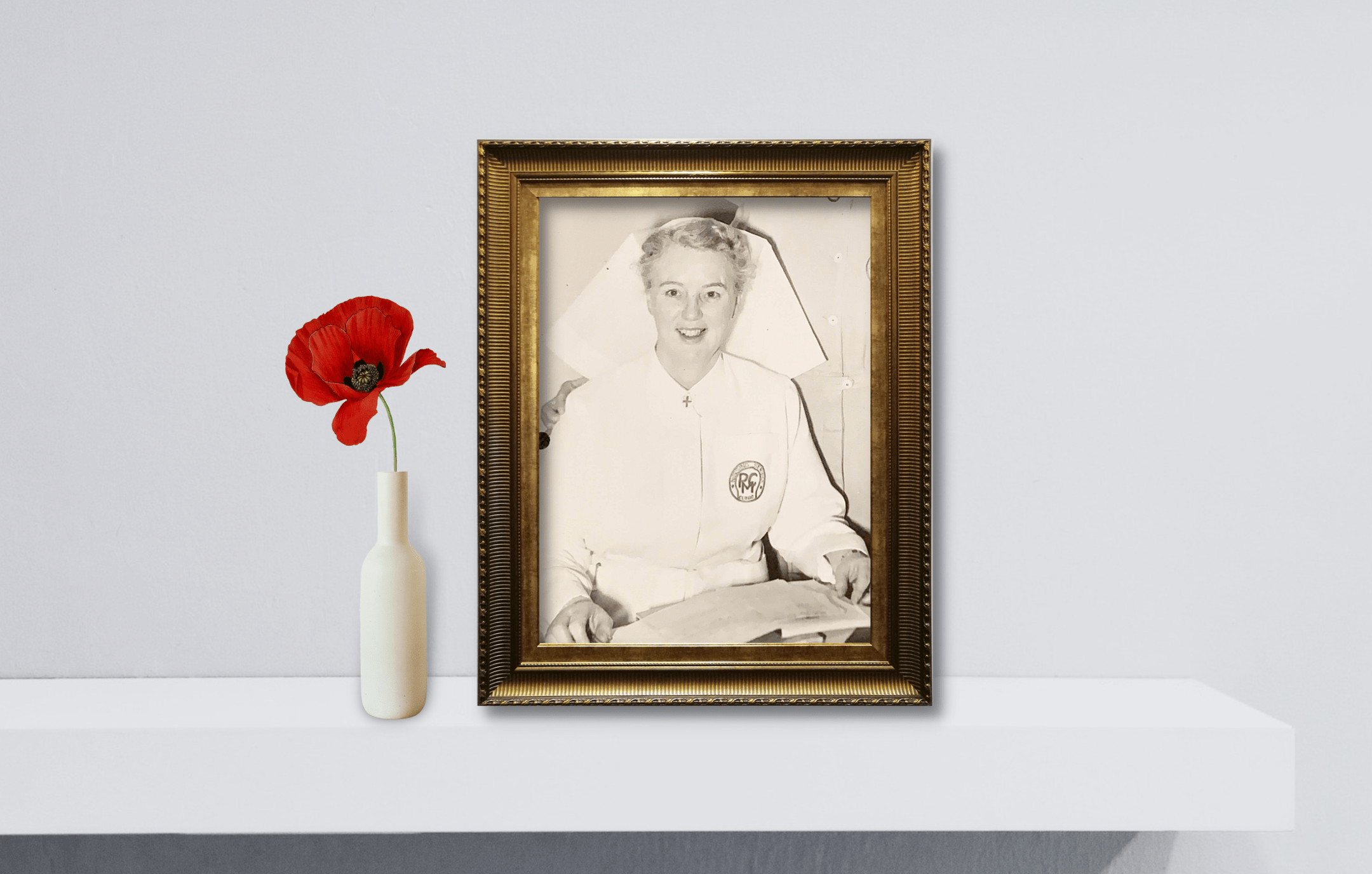
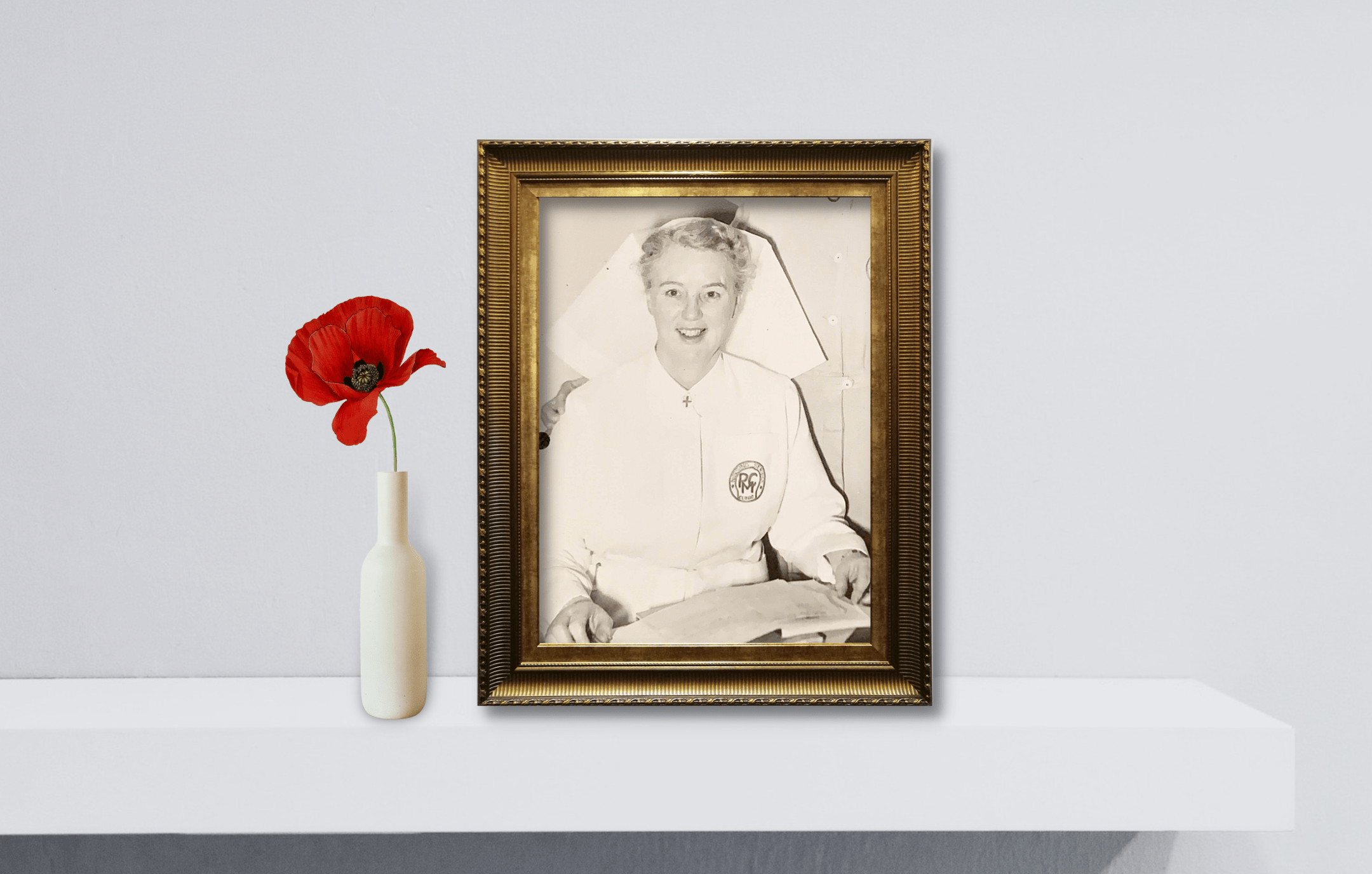
She dedicated her later life to caring for cancer patients, but Peter Mac Matron Nancie Kinsella’s nursing story began on the battlefields of World War II.
On April 15, 1945, British forces entered Belsen Concentration Camp in northern Germany and discovered the horrors that had been taking place there. They found thousands of prisoners close to death.
Nancie Kinsella was one of an enormous team who worked tirelessly around the clock to provide medical care, food, and water to the 1700 survivors. They faced an uphill battle against disease, with dysentery, tuberculosis, typhus, diphtheria, heart and kidney problems, and the devastating effects of starvation.
An estimated 50,000 people had died there.
Fifteen years earlier, a fresh-faced Kinsella was completing her nursing training in Melbourne, working first as a nurse and then a midwife.
In 1936 she took a voyage across the world to work in Rhodesia and South Africa before making her way to the United Kingdom.
She was nursing in England when the Second World War broke out and she would soon be catapulted into horrors she could have never imagined.
She enlisted in the Queen Alexandra’s Imperial Military Nursing Service, her first posting was the Middle East before being sent to Normandy where she looked after D-Day casualties.
She was then sent to Belsen. In the weeks following the liberation, the British army arrested and tried the camp’s administrators and guards, many of whom were sentenced to death for their crimes.
Nancie was appointed Member of the Order of the British Empire (MBE) in recognition of gallant and distinguished services in North West Europe and was awarded the Associate Royal Red Cross (ARRC) for acts of bravery or exceptional devotion to duty.
She remained in the service and completed her time in the Reserve of Officers in 1956 before returning to Australia and then Peter MacCallum Cancer Centre.
She was the matron of Peter Mac from 1956 to 1967 and was responsible for establishing Australia’s post grad Radiotherapy Nursing Course.
The Nancie Kinsella Patients’ Library was created in her honour by her fellow nursing staff, opening in 1968.
The library is celebrating its 55th anniversary in 2023.
Nancie Kinsella was a war hero and a practice-changing nurse who built the foundations of oncology nursing in Australia. Lest we forget.

- Details
- Written by: Nadia Joulian
- Category: News
- Hits: 244
Two Peter Mac Medical Oncologists and Researchers presented the results of exciting first in human trials in bowel cancer and solid tumours at the prestigious American Association for Cancer Research Meeting.

Professors Jayesh Desai and Ben Solomon from Peter Mac shared their experience of leading trials with new therapies that target RAS, the most commonly mutated pathway in cancer.
“Early results of a trial with GDC-6036 (now known as divarasib -a new KRAS targeted treatment) combined with cetuximab in patients with bowel cancer look very promising with 62 per cent of patients having a significant response to treatment,” said Professor Jayesh Desai, Associate Director of Clinical Research at Peter Mac.
“KRAS is one of the most commonly mutated pathways in cancer. We have been successful in developing treatments that target a unique type of KRAS mutation called KRAS G12C that is of particular importance in bowel and lung cancer,” said Professor Desai.
“These treatments have been successful in lung cancer but finding a treatment that works in bowel cancer has been more challenging until now.
“Bowel cancer affects about 15,000 Australians each year and can be very challenging to treat if it is not caught early, which is why this new treatment is very exciting,” he said.
“In this global trial, presented by lead investigator Professor Desai from Peter Mac, we tested the new treatment called divarasib which very potently targets KRAS G12C, along with an approved drug cetuximab, which targets a key protein in bowel cancer known as EGFR.
“We are encouraged by these results and look forward to conducting more research to further assess the safety and benefits of this treatment,” said Professor Desai.
In the same special session on clinical use of KRAS inhibitors, Peter Mac clinician researcher Professor Ben Solomon presented his experience of using the RAF dimer inhibitor called lifirafenib in combination with the MEK inhibitor mirdametinib in patients with advanced or refractory solid tumours, with encouraging initial results seen in a number of tumour types.
Also presenting at the American Association for Cancer Research Meeting was Dr Heidi Fettke who presented data on genomic aberrations in circulating tumour DNA in metastatic castration-resistant prostate cancer and Professor Sarah-Jane Dawson was invited to present on liquid biopsy opportunities and challenges of Cell-Free DNA.
International meetings of this calibre allow our researchers to share ideas, collaborate and showcase the depth of research coming from Peter Mac.
Professors Jayesh Desai and Ben Solomon from Peter Mac shared their experience of leading trials with new therapies that target RAS, the most commonly mutated pathway in cancer.
“Early results of a trial with GDC-6036 (now known as divarasib -a new KRAS targeted treatment) combined with cetuximab in patients with bowel cancer look very promising with 62 per cent of patients having a significant response to treatment,” said Professor Jayesh Desai, Associate Director of Clinical Research at Peter Mac.
“KRAS is one of the most commonly mutated pathways in cancer. We have been successful in developing treatments that target a unique type of KRAS mutation called KRAS G12C that is of particular importance in bowel and lung cancer,” said Professor Desai.
“These treatments have been successful in lung cancer but finding a treatment that works in bowel cancer has been more challenging until now.
“Bowel cancer affects about 15,000 Australians each year and can be very challenging to treat if it is not caught early, which is why this new treatment is very exciting,” he said.
“In this global trial, presented by lead investigator Professor Desai from Peter Mac, we tested the new treatment called divarasib which very potently targets KRAS G12C, along with an approved drug cetuximab, which targets a key protein in bowel cancer known as EGFR.
“We are encouraged by these results and look forward to conducting more research to further assess the safety and benefits of this treatment,” said Professor Desai.
In the same special session on clinical use of KRAS inhibitors, Peter Mac clinician researcher Professor Ben Solomon presented his experience of using the RAF dimer inhibitor called lifirafenib in combination with the MEK inhibitor mirdametinib in patients with advanced or refractory solid tumours, with encouraging initial results seen in a number of tumour types.
Also presenting at the American Association for Cancer Research Meeting was Dr Heidi Fettke who presented data on genomic aberrations in circulating tumour DNA in metastatic castration-resistant prostate cancer and Professor Sarah-Jane Dawson was invited to present on liquid biopsy opportunities and challenges of Cell-Free DNA.
International meetings of this calibre allow our researchers to share ideas, collaborate and showcase the depth of research coming from Peter Mac.
- Details
- Written by: Nadia Joulian
- Category: News
- Hits: 160
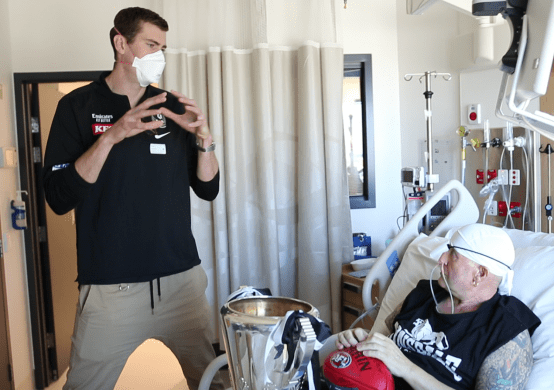
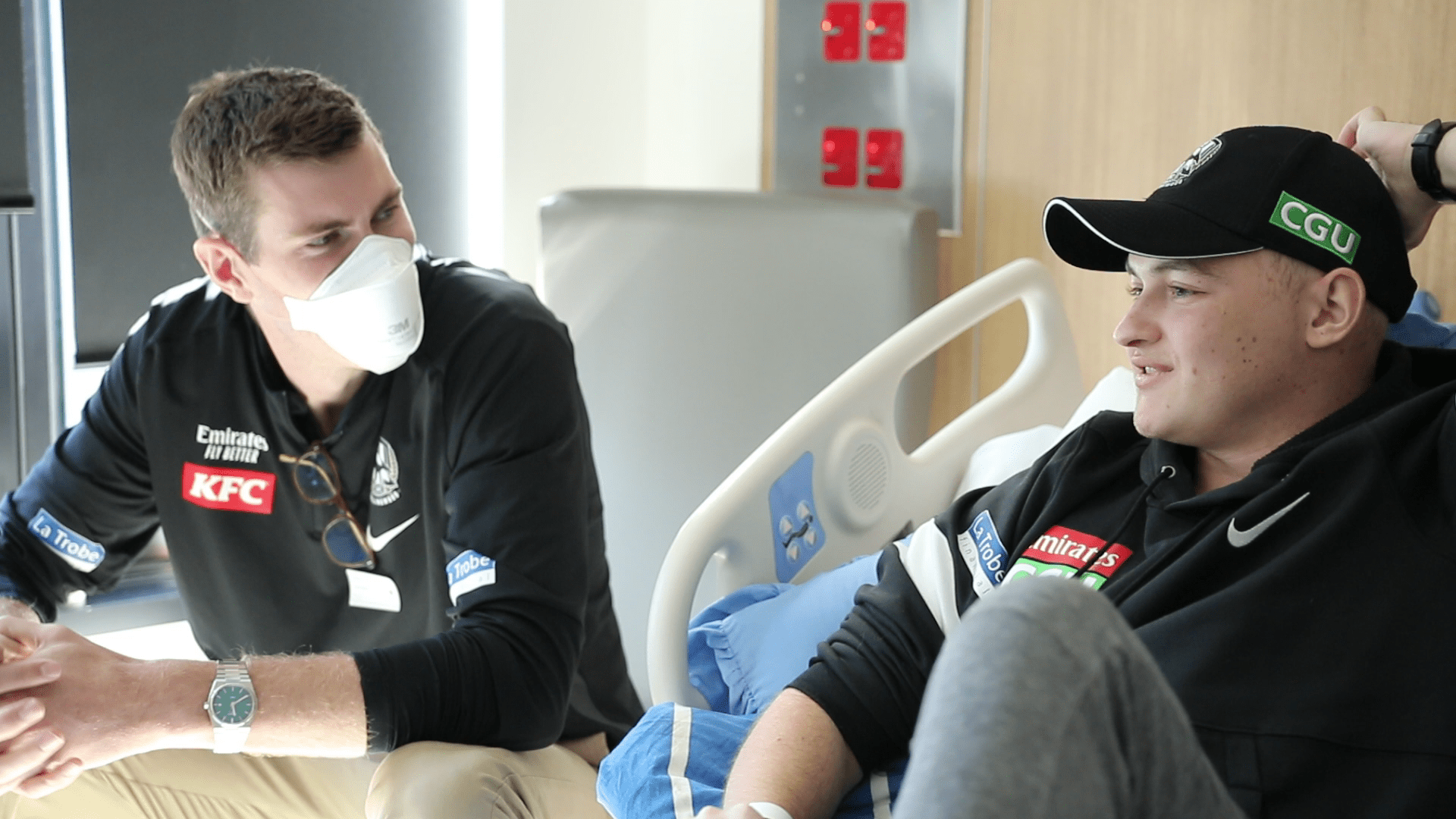
Proving he also has a big heart, Collingwood's Mason Cox dropped in to Peter Mac today to visit some of our patients.
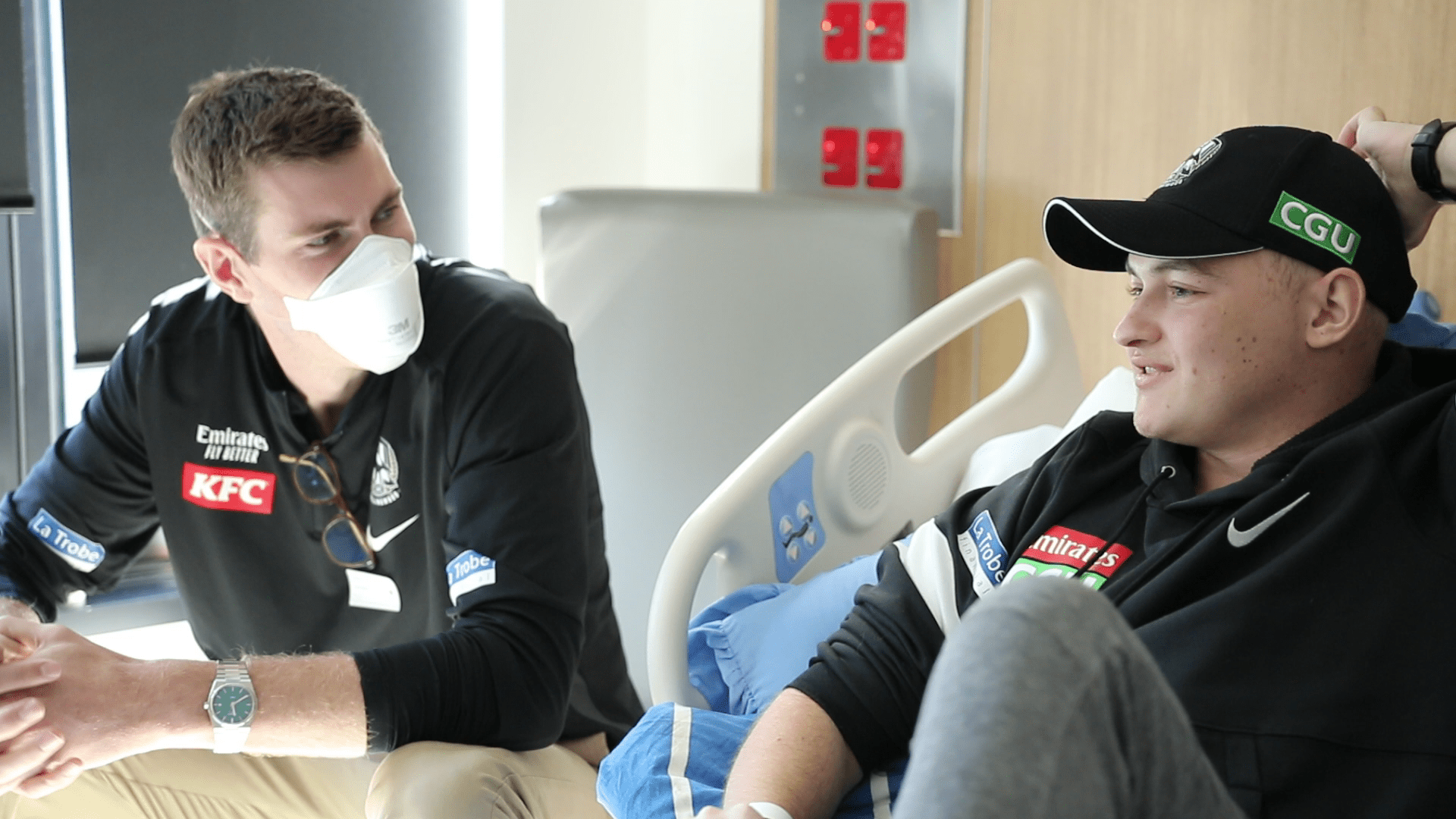
Peter Mac patients (and massive Collingwood fans!), Nick and Ricky, had the chance to meet one of footballs tallest heroes and to hold the 2010 AFL Premiership Cup.
A huge thank you from Peter Mac to Mason and everyone involved at @collingwood_fc.
The visit not only meant the world to Nick and Ricky but also made the day of our staff