
- Details
- Written by: Naomi Harrison
- Category: News
- Hits: 235
We interviewed Hayley Beer, Clinical Nurse Consultant in the haematology stream to understand more about her role and the value of nurse led research to improve patient outcomes.

How long have you been at Peter Mac?
Been at Peter Mac since: I started at Peter Mac in 2017 but I had been working at the Royal Melbourne Hospital since 2004 in the oncology team.
Tell me a little bit about your role and what you are about to embark on:
I am a Clinical Nurse Consultant working in the Myeloma and Autograft stream. My clinical work includes patient and family preparation for complex therapies; assessment and management of disease and treatment-related side-effects and survivorship care. As a Nurse Consultant, research is also a key component of my role and a passion of mine. I am looking forward to embarking on my Master of Philosophy at Melbourne University in Graduate Research this year.
Building research capability among clinical nurses is essential to the delivery of safe and efficient care. My interest in nurse-led research started with a project I was working on to teach patients to self-inject subcutaneous therapy at home. Patients would sometimes spend all day travelling into Peter Mac, waiting for their appointment to receive an injection that would take 30 seconds. I had come to really understand and appreciate how important time was for these patients living with an incurable cancer and wanted to find a way to help them spend more time with loved ones and family, rather than in the hospital.
I set up a simple but impactful study to survey patients about their view regarding home or hospital-based administration of the injection and 80 percent said they would be happy to do the injection themselves at home. This led to the development of a nurse-led model of care that included teaching patients how to inject and manage any side effects and symptoms associated with the subcutaneous therapy, remotely. Because this innovation was in place before the pandemic hit, it allowed a lot of patients to stay home without compromising their care. The nurse-led service resulted in removing three out of four hospital visits for patients.
I am really proud that my research has a tangible and timely impact on patient care, and has driven me to explore other opportunities for nurse-led research. I am particularly interested in improving patient experience by examining the impact treatments have on quality of life for patients in real-world settings. This will take into account social determinants of health and what matters most to patients to ensure they have the best experience and outcomes of care possible. I recently completed a study with colleagues from the Academic Nursing Unit (Holly Chung, Mei Krishnasamy). We asked people living with myeloma to review ten commonly used patient reported outcome measures (PROMs) to help us better understand which suites of measures comprehensively capture what matters most to them regarding their quality of life. We now have a collection of three PROMs endorsed by patients for use in future studies. I have recently submitted a manuscript for publication reporting on this Australian first collaborative study.
Nurse-led research is under-resourced and under-represented nationally and internationally, but at Peter Mac, we are making inroads to address this significant gap. I’m so grateful for the support and encouragement of Professor Mei Krishnasamy who has really inspired me to progress this pathway and I hope I can encourage other nurses to do the same.
What do you enjoy most about your role?
I really enjoy the flexibility to care for patients at any time point, whether it is at home or in the ward, getting to know the family and carers. As a Nurse Consultant you get to build relationships, see things through and find ways to make the experience of care and living with incurable cancer better for patients. Nurses are essential members of a patient’s multidisciplinary team. They bring a different but complimentary insight to a patient and family’s needs, and that mix of insights is key to delivering the best outcomes possible.

- Details
- Written by: Naomi Harrison
- Category: News
- Hits: 86
Dawn is a veritable knitting machine – in fact, she pumps out hundreds of one-off designs to raise money for Peter Mac every year.

This week, Dawn (left in the photo with her daughter Shona) brought her latest haul of gorgeous toys to Peter Mac in preparation for Wednesday's Easter stall, run by Volunteer Services.
It appears there’s nothing she can’t knit – there’s popular characters from children’s stories, bears, dragons and even baby chicks that pop out of knitted eggs.

Dawn made a pledge to do all she can to raise money for cancer research – she lost her husband to cancer and her family has been touched by it many times.
“It really gives me so much joy when I’m knitting knowing that it will raise money for something important. That really drives me,” Dawn explains.
“I also love having a theme and a collection to knit, so my daughter and I have had a lot of fun selecting Easter designs - we hope people enjoy them as much as I’ve enjoyed knitting them.”
Dawn is one of an army of volunteers who provide beautiful hand-made items for Volunteer Services – all proceeds going to support important projects across Peter Mac.
“We’re incredibly lucky to have so many dedicated supporters – and their talent is absolutely mind blowing,” Volunteer Services Manager Anna Taylor says.
“Dawn is such a talent – it’s hard to believe that these are hand-made, they’re so perfectly finished – we know they’ll be snapped up quickly.”
The Volunteer Services Easter stall will be on Wednesday April 5 from 10:30am to 3:00pm in the Welcome Hall.
- Details
- Written by: Naomi Harrison
- Category: News
- Hits: 129
Researchers found that, despite being heavily immunocompromised, haematology patients generate strong cellular immune responses against SARS-CoV-2 after vaccination, on par with that of healthy individuals.
Published today in Cell Reports Medicine, the research team, led by University of Melbourne Professor Katherine Kedzierska, a Laboratory Head at the Peter Doherty Institute for Infection and Immunity (Doherty Institute), undertook the most comprehensive analysis of adaptive SARS-CoV-2 immunity to date in haematology patients of varying diseases and treatments across three doses of COVID-19 vaccination in comparison to healthy individuals.
The research was performed in collaboration with Associate Professor Benjamin Teh, Professor Monica Slavin and Professor Constantine Tam from the Peter MacCallum Cancer Centre. Associate Professor Teh says this research is important for clinicians working with blood cancer patients.
“Clinicians can be confident that it is safe and beneficial for their patients, who are heavily immunocompromised and vulnerable to severe COVID-19 infection, to receive vaccination against SARS-CoV-2. Regardless of their diseases and treatments, COVID-19 vaccination generates strong T cell immunity in this group,” Associate Professor Teh says.

University of Melbourne Dr Oanh Nguyen, Senior Research Fellow at the Doherty Institute and co-lead author of the paper, says it is important to really understand vaccine efficacy in this immunosuppressed high-risk group of patients to help prevent severe SARS-CoV-2 infection.
“This group is at high risk of viral infectious diseases, such as influenza and SARS-CoV-2, and yet they are not always included in pre-clinical trials that test vaccine efficacy,” Dr Nguyen says.
“Our study shows that they highly benefit from receiving three doses of vaccination. The vaccines boost their levels of T cells, the white blood cells that kill viral infected cells, irrespective of the patient’s B-cell numbers and antibody response.
“We also looked at the characteristics of these T cells that are generated after vaccination, and we found that these signatures are very similar to healthy individuals that are either infected or vaccinated. These findings are really important and super exciting for cancer patients,” Dr Nguyen adds.
Professor Kedzierska says that the study provides key insights for future immunisation strategies with vaccines such as influenza which predominantly induce B cell immune responses.
“What we have shown is that people with co-morbidities that have a heavily impacted B cell immune arm, can have an mRNA vaccine to elicit T cells and give them that extra level of protection,” Professor Kedzierska says.
Media Enquiries:
To arrange an interview, call the Peter Mac Communications team on 0417 123 048 or Aline Riche, Senior Media and Communications Officer, at the Doherty Institute on 0403 204 336.

- Details
- Written by: Naomi Harrison
- Category: News
- Hits: 115
Peter Mac has welcomed four recent graduates into the Psychosocial Oncology team, boosting our capacity to support the emotional and psychological needs of patients and families.
Dr Olivia Chung, Jardine Mitchell, Jake Garvey and Ana Lea have commenced their work with patients over the last few weeks.
Head of Clinical Psychology Dr Elizabeth Barson explains, “We are lucky to have attracted such high calibre candidates, who are energetic and passionate about how good mental health contributes to good physical health.”
Peter Mac’s inaugural Psychosocial Oncology Registrar Program is supported by the Victorian Department of Health, with funding secured for three two-year positions per year over the next three years.
Elizabeth explains, “This funding allows us to significantly increase our reach across the organisation and provide more timely and flexible care.”
Each of the new team members are passionate about supporting patients and families throughout the cancer journey, with their areas of interest ranging from working with older adults, adolescents and young adults, LGBTQIA+ communities, cancer survivorship, and supporting patients receiving palliative care.
They are all looking forward to rotations through different work areas, the opportunity to work closely with several muldisciplinary nursing and allied health teams, and the supported learning offered by senior team members to help them further develop their skills.
In reflecting on program Ana Lea said, “I aim to support patients living with a cancer diagnosis by witnessing and facilitating their strengths, inherent problem-solving abilities, and reflecting on what is important to them.”
Of our four new recruits, Jake Garvey, Jardine Mitchell and Olivia Chung are already familiar with Peter Mac, having completed placements with our Psychosocial Oncology Program during their studies.
Olivia describes her previous Peter Mac experience as, “an incredibly humbling and formative experience in my early career and I am thrilled to be returning to complete my registrar program.”
Learn more about Peter Mac’s Psychosocial Oncology supports and services here.
- Details
- Written by: Naomi Harrison
- Category: News
- Hits: 85
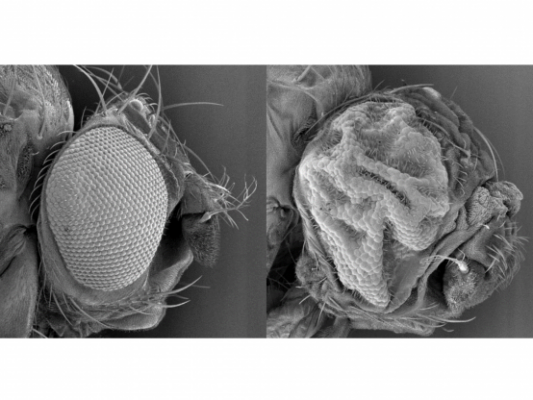
They might be known colloquially as the ‘fruit fly’ but the Drosophila fly is a very different breed to the agricultural pest.
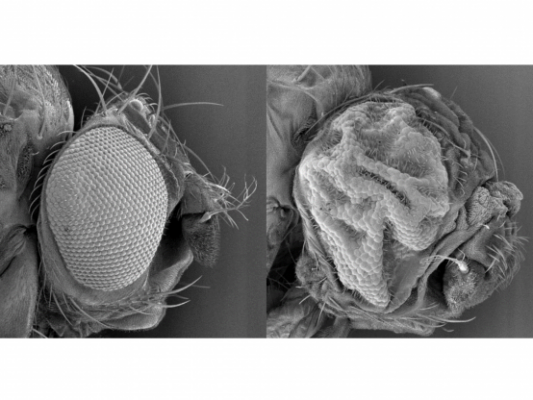
The Drosophila fly is used to help us understand many human diseases and has already facilitated an inordinate number of discoveries from heredity, body patterning, circadian rhythms, innate immunity, and cancer signalling pathways.
“The formation of the Australian Drosophila Transgenic Facility will enable researchers to genetically modify the fruit fly and remove specific genes, or overexpress genes allowing us to study human diseases,” said Professor Kieran Harvey, Group Leader of the Organogenesis and Cancer Program at Peter Mac.
“Drosophila is a particularly good model to study human diseases because seventy percent of human disease genes have a counterpart in the fly, and they are also much faster and cheaper to work with than other animal models.
“This facility will mean that any Australian researcher can manipulate the genome of Drosophila to answer fundamental research questions right here in Australia,” he said.
“Bringing this capacity and skill set to our shores reduces the cost and increases the speed of research. It also enhances a researcher’s ability to manipulate more genes, allowing a broader application of the fly model.”
Associate Professor Louise Cheng and Professor Harvey will co-lead the facility that is supported by Phenomics Australia and Peter Mac and will service researchers around Australia with their Drosophila transgenesis requirements.
Associate Professor Cheng said her team use Drosophila as a model organism to investigate several things including how tumours can grow at the expense of muscles and adipose tissue during cancer when the body wastes away.
“This new centre will save us from having to send our gene modification requirements to the USA and wait for the fly model to be returned.
“I am excited by the possibilities and increased research avenues this will open up for us,” she said.
Many of the key cancer signalling pathways were first discovered in Drosophila, such as Notch, Hedgehog and Hippo, along with key components of other pathways such as the RAS/MAP kinase pathway.
These discoveries have led to new therapies and avenues for treating cancer.
The humble Drosophila fly has been responsible for at least five Nobel prize winning discoveries and maybe the next one will come from research facilitated by the Australian Drosophila Transgenic Facility at Peter Mac.
If you would like to use the services of the Transgenic Fly Lab please reach out to Kieran Harvey
