
- Details
- Written by: Nadia Joulian
- Category: News
- Hits: 12
{SLIDER}
This is a new change I want to make! Test
corrected

- Details
- Written by: Mandi Robertson
- Category: News
- Hits: 158
Entering a clinical trial for cancer treatment can be a complex decision for patients.
The Parkville Cancer Clinical Trials Unit (PCCTU) worked with the Health Services Research Team at Peter Mac to uncover ways to improve patient communication and help them navigate this decision.
“The research highlighted that having both comprehensive verbal and written information was important to patients entering a trial for the first time,” said Amelia Hyatt, Senior Research Officer, Health Services Research.
“Many patients did not fully understand trial eligibility with information about randomisation difficult to interpret and a barrier to enrolment for some.
“Patients who were already on trials felt their care was exceptional however transitioning off a trial was an adjustment as they moved to less intense clinical care and there was the worry of spending time on a trial if the treatment was not deemed effective.” Ms Hyatt said.

The PCCTU Manager Marian Lieschke said they undertook the research project to truly understand the complexities of communication with patients already on trials or about to enter a trial to find areas that they could improve.
“We have already implemented changes based on the research findings such as a new team member who is dedicated to helping patients transition off a trial,” Marian said.
“Another area we are working to improve is the handover between the tumour stream clinical nurse consultant and the PCCTU team.
“We are developing an electronic medical record tool for this to ensure there is a continuity of care this will also ensure the knowledge of the patient journey is not lost as they move from standard clinical care to trials and back again,” Marian said.
The research also highlighted that patients are very satisfied with their trial management through the PCCTU overall and small tweaks can make the service and their experience even better.
The research was published in Biomedical Central (BMC) and in was a team effort involving Amelia Hyatt, Dr Rowan Forbes Shepard and Ashleigh Bradford from the Department of Health Services Research.
- Details
- Written by: Christopher Talbot
- Category: News
- Hits: 658

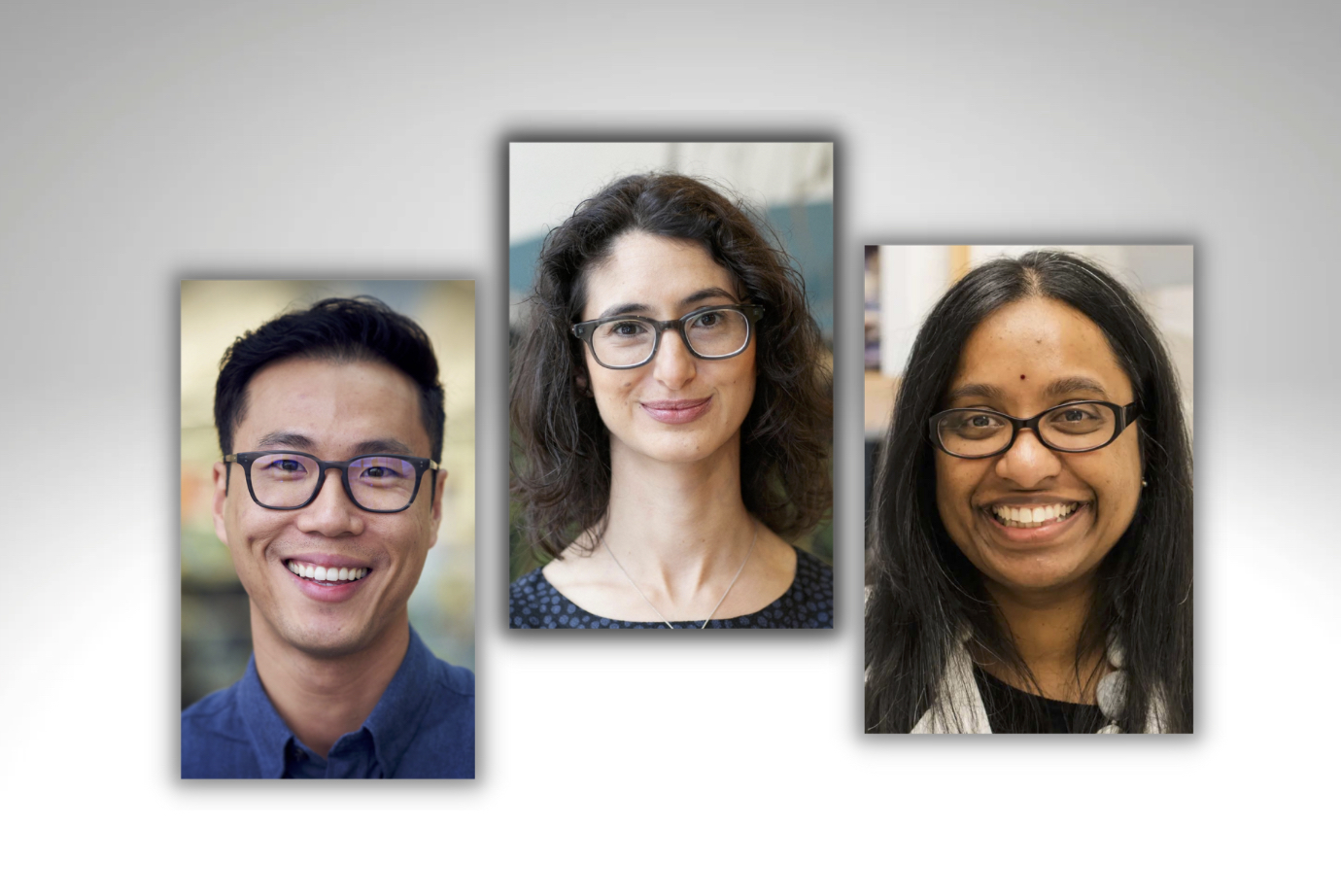
Three of Peter Mac’s most promising clinical researchers have received 2023 Discovery Partner Fellowships.
The 2023 Fellowships, generously supported by the Peter Mac Foundation, have been awarded to Dr Aparna Rao, Dr Julia Dubowitz and Dr Lewis Au.
“We are very proud of this program and the outcomes our Discovery Partner Fellowship recipients have achieved in the past,” Associate Director, Clinical Research, Professor Jayesh Desai said.
“The Fellowship provides time away from front-line clinical roles to progress defined research projects focussed on advancing cancer treatments and improving patient outcomes and experience.
“This year we had many extraordinarily strong candidates. All underwent a competitive evaluation process to enable us to select just three recipients,” he said.
Kate Torney, Executive Director Foundation, said they are proud to support this important program.
“It’s amazing to think that more than 50,000 Australians, who give so generously to our Discovery Partner program each month, are empowering researchers to make such remarkable progress in cancer research, right here at Peter Mac,” she said.
Read more about each research project below.
Dr Aparna Rao - Identification of metabolic phenotypes associated with prognosis and therapeutic response in patients with melanoma (The MetaMel Study)
Australia has the highest incidence of melanoma globally. Although newer therapies have dramatically improved outcomes, we have limited understanding of why some patients relapse or do not respond to therapy. Understanding the fuels that tumours use to derive energy (metabolism) could potentially help answer such questions.
Dr Rao will use novel techniques to characterise metabolism in living melanoma tumours. She will use recently developed ground-breaking techniques to study metabolism directly in patients rather than using pre-clinical models in the laboratory.
This exciting opportunity will allow us to gain insights into tumour metabolism in a manner that was impossible in the past. The two main techniques to be used involve assessing characteristics of the metabolism of a tumour from a standard biopsy sample (using a method known as metabolomics) and administering a non-radioactive, stable isotope infusion of glucose, to get a detailed view of how melanomas utilise this important fuel to aid their growth.
Dr Rao aims to apply the knowledge gained from these studies to develop biomarkers to predict which patients are likely to relapse and help develop novel therapies for patients with melanoma.
Dr Julia Dubowitz - Modulating the perioperative stress response to improve patient outcomes after cancer surgery
Surgery remains the primary treatment for many solid cancers, but major surgery places the body under significant stress. Furthermore, complications after major cancer surgery can occur in up to 25 per cent of patients. These complications can delay or impair a patient’s recovery, quality of life and importantly, their ability to receive other life-saving cancer therapy.
Anaesthesia (administered to facilitate surgery) alongside other treatments at the time of surgery plays a role in modulating the extent of this deleterious stress response.
Dr Dubowitz’s research aims to investigate the effect of surgical stress on patients undergoing major cancer surgery. She aims to identify potential therapeutic targets around the time of surgery to reduce post-surgical complications and improve long-term cancer survival.
Dr Lewis Au - Developing a spatially-stable predictive biomarker of immunotherapy response in clear cell renal cell carcinoma
Immunotherapy is now a standard treatment for many patients with cancer. In particular, for patients with stage IV kidney cancer, immunotherapy can provide initial responses in 50-60 per cent of cases. However, accurate selection of patients for immunotherapy is difficult as there is no way of knowing who is best suited to this treatment or will derive longer term benefits.
This is particularly challenging in kidney cancers, which are often made up of different populations of cancer cells even within a given tumour or metastasis, almost like a mosaic. This is termed ‘intratumour tumour heterogeneity’. Therefore, a biopsy of one area to do molecular testing may give a different result to another area – and doing multiple biopsies for patients is not a practical solution.
Dr Au’s project leverages his previous work that showed a new RNA-based assay can help, where one biopsy can accurately capture the total intratumour heterogeneity of kidney cancer, with potential for this to be implemented in clinic in due course. He aims to apply this technique first to find out what the signature is for kidney cancer and how this relates to immunotherapy response, then validate this finding using tumour material collected as part of the ongoing KRAB Kidney Cancer Registry running at Peter Mac and other sites in Victoria.
The goal is ultimately to develop a test that can be used in clinic, to understand upfront who is best suited to immunotherapy treatments in order to better personalise care for patients with this disease.
Now in its sixth year, the Discovery Partner Fellowships program is open to early or mid-career Peter Mac clinicians who also perform research.
The Fellowship provides financial support and a mechanism to carve out time from clinical roles (between 0.2 and 0.3 FTE) to progress well-planned research projects.
Congratulations to the three very worthy recipients. We look forward to observing the outcomes of your research as you strive to improve outcomes for cancer patients.

- Details
- Written by: David Walsh
- Category: News
- Hits: 856

Peter MacCallum Cancer Centre and The University of Melbourne will establish a new centre to transform how genomics and precision oncology is delivered in Australia.
The model will be unique in the Asia Pacific region, bringing together Peter Mac and The University of Melbourne’s world-leading cancer, genomics and precision medicine experts into a unified group.
The centre will deepen collaboration across these specialities and encourage new joint research initiatives in the discovery-phase and clinical application of genomics. It will become a focal point in the cancer care landscape, forming strong connections with global clinical trial networks and industry.
A memorandum of understanding (MoU) to establish the centre and formalise how Peter Mac and The University of Melbourne will work closely together over the next year was signed today.
University of Melbourne is the highest ranked Australian university across the three major global rankings, while Peter Mac is Australia’s only public health service dedicated to caring for people with cancer.
Peter Mac Chief Executive, Professor Shelley Dolan said the two organisations have a long history of collaboration, with a shared vision of enhancing patient access to evidence-based cancer care.
“We’re excited to be embarking on a mission to increase the scale, capacity and reach of precision cancer care in Victoria,” Professor Dolan said.
“It will mean more patients, including those in regional areas, will have access to this service which is critical in terms of the treatments they receive and for their outcomes from cancer.”
Genomics involves patients undergoing a genetic test and using this information to personalise their care. It often enables patients to be diverted to treatments most likely to work for them, avoiding potential toxicities and time lost to treatments less likely to work.
Key aims of the new centre will be to:
- Establish novel genome diagnostic referral services for patients with unmet needs
- Close the gap in regional access to genomics by increasing the number of delivery models and expert services
- Broaden and co-develop genomic and bioinformatic research capability and infrastructure for cancer discovery and genomic medicine
- Drive precision oncology clinical implementation across Peter Mac, Victoria and nationally.
Dean of Medicine, Dentistry and Health Sciences at the University of Melbourne, Professor Jane Gunn, said “Coming together to share knowledge and resources can improve the lives of people with cancer by increasing our capacity to advance genomic innovation, offer precision medicine and deliver effective new therapies and prevention strategies.”
“This collaboration will advance our knowledge and capability, enabling more people to access high-quality treatment, improving equitable access to health care for those who need it most.”
